Candida albicans is a yeast that occurs naturally in and on the body. It does not usually cause problems, but if circumstances change then the candida can grow and cause a candida infection. Most candida infections are innocent and will disappear by themselves. However, when a candida infection does not pass or keeps coming back, it needs to be treated.

Candida
Treatments
- All treatments
- Prescription medicines
- Non-prescription medicines
- Relevance
- Name A-Z
- Name Z-A
- Price low-high
- Price high-low
How does Dokteronline work?
At Dokteronline, you can get expert advice from doctors quickly, without the hassle of visiting your GP’s surgery. Take care of your health with reliable treatments and information from the comfort of your home.
Select your preferred treatment
The doctor will review your medical request
The pharmacy will ensure your medication is delivered to your doorstep
What is candida?
Candida is a fungal infection caused by yeasty fungi. The most common yeast in humans is candida albicans, which flourishes in a warm and humid environment. Candida albicans can be found on the skin, in the skin folds and on the mucous membranes of the mouth, oesophagus, intestines and genitals. In healthy people, this fungus does not normally cause any symptoms. Due to various factors however, this yeast can form threads, which are then considered to be a candida fungus.
What are the causes of candida infections?
There are causes that apply to all forms of candida and there are local causes. The general causes are:
- Medication such as antibiotics, that kill bacteria but not the candida yeast;
- The contraceptive pill, which causes fluctuations in the hormone balance that seems to affect the growth of candida;
- Chemotherapy, which can reduce resistance;
- Serious diseases that also reduce resistance, such as cancer, being HIV positive, having undergone a transplant;
- A lack of vitamin B or iron;
- Diabetes.
The reason why people with diabetes are more likely to have a candida infection is not yet entirely clear. A reduced resistance could be a cause, or in the case of candida of the skin, the thought is that the small blood vessels deteriorate and the skin becomes more vulnerable as a result. The local causes can differ depending on the type of candida, which are outlined below.
What forms of candida infections are there?
A candida infection can develop on various parts of the body:
- The mouth
In addition to the general causes, the candida infection can be caused by inhalation of medication, intubation during surgery, abrasion of poorly fitting dentures, smoking and dry mouth by medication.
- The oesophagus
A candida infection of the oesophagus can be caused by inhalation of medication (corticosteroids in cases of asthma), intubation during surgery and smoking.
- The vagina
In addition to the general causes, hormone fluctuations during pregnancy and due to the pill can cause a candida infection, as can an incorrect PH value due to soap.
- The penis
A candida infection of the penis is not common, but can be caused by a tight foreskin or by a transfer from a partner who has candida. Candida is not a sexually transmitted disease, but it can be transmitted.
- The skin and skin folds
This type of candida infection occurs when the skin becomes irritated or damaged by, for example, too much soap use or rubbing against the clothing. Candida thrives in warm and moist spots such as the skin folds, and people who are overweight are more likely to suffer because of the larger skin folds.
- The nipples
During breastfeeding, the nipple is a warm and humid place where candida can easily develop. Breastfeeding is likely to damage your nipple during feeding, while your baby’s moist mouth is also a risk factor in itself. Your baby can also have a candida infection (thrush). Hormonal fluctuations during pregnancy and after childbirth can also play a role in the development of candida.
- The nails and the edges of the nails
These will likely be the first point of contamination of the skin by candida. Public spaces such as swimming pools are a risk in the case of lime nails. The cuticle can be damaged by a lot of water (softening), as well as nail biting and picking. The candida can get into the damaged areas and cause an infection.
- The corners of the mouth
In addition to the general causes of candida, cracks in the corners of the mouth can also be caused by poorly-fitted prostheses or artificial teeth that are not at the right height.
- Generalised candida
In rare cases, candida ends up in the blood. This form occurs in people with a strongly reduced resistance.
How do you recognise candida?
The symptoms of a candida infection depend on the location.
Mouth (thrush)
- White dots, which together can form larger areas (plaques) that can be coloured grey or yellowish;
- Sores;
- Swollen spots if dentures are the cause;
- Pain when swallowing.
Oesophagus
- Difficulty swallowing (the main complaint) of both solid food and liquid also of water or saliva;
- Pain near the sternum that can radiate to the back or shoulder blades;
- Frequent yellowy -white deposits in the oral cavity and on the tongue.
Vagina
- Itching, sometimes on the labia;
- White, not strong-smelling, sometimes crumbly discharge;
- Occasional red, swollen and painful mucous membrane of the vagina;
- Occasional burning or painful sensation when urinating or having intercourse.
Penis
- Itching;
- Redness of the foreskin, perhaps swollen on the inside;
- Pain when urinating;
- Pain during intercourse.
Skin
- Red spots with flakes on the edges;
- Ringworm;
- Itching, burning sensation;
- Pimples and blisters.
Nails
Thick, crumbly, yellow nails.
Nail tip (paronychia)
Red, painful and swollen skin on both sides of the nail.
Corners of the mouth (angular cheilitis)
Painful, potentially itchy cracks
Nipples during breastfeeding:
- Redness and/or soreness with a burning sensation;
- Damage or fissures;
- White dots in the skin folds;
- Serious itching;
- Skin and areola become smooth and tense;
- Severe stabbing pain in the breast during and after breastfeeding, potentially radiating to the shoulders and back.
Babies can also have candida (thrush) with symptoms such as white cervical spots on the oral mucosa and tongue, a white deposit in the mouth and tongue and often a shine on the lips.
Generalised:
Severe illness and high fever.
Is there anything I can do to fight candida infections?
Good hygiene is key. Do not use soap – dab the areas where you have candida and keep them as dry as possible. Ensure good oral hygiene in candida of the mouth, corners of the mouth and oesophagus. Avoid very hot drinks or food, acidic products, strong spices and alcohol in the case of candida of the oesophagus. For all candida infections, try to increase your resistance by living healthily with a varied diet, by not smoking and consuming little or no alcohol. Drink plenty of water, avoid stress, sleep well, exercise regularly and ensure sufficient relaxation.
What are the forms of treatment?
A candida infection can pass by itself. Your doctor may use any current medication you are taking, such as antibiotics, corticosteroids, the pill, and medications that have the side effect of reducing, adjusting, stopping or changing saliva production. Never do this on your own if you suspect that a medicine is the cause (or one of them) of the candida infections. Discuss your suspicions with a doctor. When inhaling medicines (such as corticosteroids), you can rinse the mouth and throat cavity with water after inhalation. Regularly clean any dental prostheses. If the candida infection does not go away or if it comes back, the doctor will usually prescribe anti-fungal medicines.
Medication
The choice of candida albicans treatment depends on the location. There are anti-fungal medicines such as gels, ointments, suspensions, creams, powders, pessaries and pills which kill the fungal cells or prevent them from growing and reproducing. If the anti-fungal medicines do not work, antibiotics may be prescribed. Sometimes a combination of medicines is given.
Always read the package leaflet before use and complete treatments as prescribed, even if the symptoms have disappeared. Only stop in the event of an allergic reaction, and contact a doctor immediately.
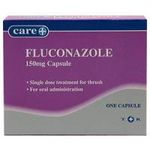
The following are the different forms of anti-fungal medicines used as candida albicans treatments:
- Miconazole;
- Clotrimazole Butoconazole;
- Fluconazole Itraconazole;
- Miconazole, which is strongest in vaginal applications, increases the effect of anticoagulants and should therefore preferably not be used in conjunction with anticoagulants.
Antibiotics that can be used as a candida albicans treatment are:
- Nystatin Amphotericin B;
- Griseofulvin suspension FNA.
Sometimes hydrocortisone can be added to a cream or ointment. It has an anti-inflammatory effect and helps against itching. Benzoic acid /salicylic acid cream or ointment can also be used on the skin.
For a vaginal candida infection, an antifungal vaginal cream, vaginal tablets or vaginal suppositories (pessaries) can be chosen. The creams can also be applied to the labia if they are itchy. For the skin folds, penis and nipples, a cream or ointment is usually chosen, while for a candida infection of the nails, the use of cream is not advised because the product does not work well in thick nails. Oral treatments are therefore preferred, while there are fungicidal nail polishes, with the treatment taking seven to 12 months. A fungicidal ointment or cream can be applied to the edges of the nails, but in case of persistent fungal infections, it is sometimes necessary to take antifungal or antibiotics for a long period of time.
For candida infections of the corners of the mouth, a zinc oxide smear can be given first to dry and protect the corners of the mouth, or a zinc oxide spread in combination with another agent. Methylrosaniline can be applied to thrush and nail edges with a cotton swab if nothing else has worked. As it can cause dark purple discolouration of the skin and can affect clothing, some people are reluctant to use it.
If a candida infection continues despite medication or if it comes back regularly, then doctors may examine the candida to see what it reacts to.
Alternative treatments
A light form of candida can also pass by itself. For your baby’s thrush, you can clean the mouth with a cloth soaked in orange juice.
Lifestyle changes
If you have a candida infection, it is important to have good hygiene. Do not use soap in places where you have a candida infection. With vaginal candida, vaginal intercourse can be painful so you can use a neutral lubricant. Avoid vaginal intercourse when the mucosa is still very dry and painful. Try not to keep your hands in water for too long (particularly fingers or cuticles) and wear gloves when cleaning, but do not keep them on too long as they may make the skin moist and soft again due to perspiration. With candida of the feet, it is advisable to wear flip-flops in swimming pools. Wear well ventilated shoes and clean socks every day. Dry your sports shoes well after exercise. For general infections, wear the clothing that is airy for the skin, preferably made of cotton.
Additional risks and side effects
Candida is not contagious, but vaginal candida can be transmitted to a sexual partner. Genital candida can also be associated with feelings of shame, which is something you may wish to discuss with your doctor. A baby can get thrush from the candida of the nipple of the mother, and vice versa. The mother can also give a candida infection to her baby during childbirth.
How can you prevent a candida infection?
A healthy lifestyle can help prevent candida. This includes food that contains sufficient iron and vitamin B, and good bodily and oral hygiene. Also, see the section entitled “Is there anything I can do to fight candida infections?” above.
Sources
Apotheek.nl. (updated on 20 09 2016). Amfotericine B. Referred to on 10 05 2019 on https://www.apotheek.nl/medicijnen/amfotericine-b#belangrijk-om-te-weten-over-amfotericine-b (Viewed on 10 05 2019).
Apotheek.nl. (updated on 15 01 2015). Medications for fungal infections of the skin. Available at: https://www.apotheek.nl/klachten-ziektes/schimmelinfecties-van-de-huid#welke-medicijnen-worden-gebruikt-bij– schimmelinfecties-van-de-huid (Viewed on 10 05 2019).
Farmacotherapeutischkompas.nl. (z.d.). Antimycotic antibiotics. Available at: https://www.farmacotherapeutischkompas.nl/bladeren/groepsteksten/antimycotische_antibiotica (Accessed on 10 05 2019).
Huidinfo.nl . (z.d.) candida of the mouth. Available at:https://www.huidinfo.nl/c/candida-mond/ (Viewed on 10 05 2019).
Isala. (23 November 2018). Patient brochure 5982 Thrush and candidiasis in breastfeeding. Available at: https://www.isala.nl/patientenfolders/5982-spruw-en-candidiasis-bij-borstvoeding/#link2 (Accessed on 10 05 2019).
Mekkes, J.R. (31-12-2016). Fungal nail Lime nail. Available at: https://www.huidziekten.nl/folders/nederlands/schimmelnagel-kalknagel.htm (Viewed on 10 05 2019).
Mekkes, J.R. (05-06-2016). Pronchya. Available at: https://www.huidziekten.nl/zakboek/dermatosen/ptxt/Paronychia.htm (Viewed on 10 05 2019).
MLD foundation (z.d.). What is candida albicans? Available at: https://www.mlds.nl/ziekten/candida-albicans-infectie-met/ (Viewed on 10 05 2019).
Sense. (z.d.). Vaginal candida. Available at: https://www.sense.info/nl/soas/soorten-soas/candida-infectie (Viewed on 10 05 2019).
Schimmelinfecties.com. (z.d.). Fungal infection of the penis. Available at:https://www.schimmelinfecties.com/soorten– schimmelinfecties/schimmelinfectie-aan-de-penis-candida-balanitis/?cn-reloaded=1 (Viewed on 10 05 2019).
Thuisarts.nl. (revised on 2 May 2016) Vaginal Fungal Infection. Available at:https://www.thuisarts.nl/vaginale-afscheiding/ik– heb-vaginale-schimmelinfectie (Viewed on 10 05 2019).